Your AI Roadmap Is Upside Down: Start With Time, Not Models



Most AI roadmaps are built upside down. They chase vendors and moonshots first, then search for value. However, in an era defined by AI-driven healthcare transformation, the scarcest input isn’t computing power; it’s time. Indeed, workforce constraints are structural. The World Health Organization projects an ~11 million global health-worker shortfall by 2030. As a result, every reclaimed minute translates directly into more patient access, higher quality, and stronger margins. Therefore, your first principle should be simple: fund minutes, not models.
This article makes the case for inverting the roadmap; therefore, leaders should prioritize use cases that reclaim time within 90 days, then scaling the same data, governance, and operating muscles across your AI portfolio. The evidence is clear, with leaders already seeing returns (a majority report meaningful ROI within year one of GenAI initiatives), regulators are approving more AI-enabled tools, and ambient documentation has become a category with measurable impact.
Key stats at a glance
- ~11M health-worker shortfall by 2030.
- 54% of leaders see GenAI ROI within year one.
- ~44% mammography workload reduction with maintained detection.
- Near-instant (≈30s) approvals in prior-auth pilots; fewer appeals/denials.
- Ambient documentation is now a distinct KLAS category with measurable clinician benefits.
1) The problem with model-first roadmaps
Model-first plans often yield scattered pilots, orphaned proofs-of-concept, and limited clinical adoption. Meanwhile, the everyday math is unforgiving. Physicians spend significant after-hours “pajama time” finishing charts and inbox work, and many specialties still log hours of EHR effort outside scheduled clinic, lost capacity, burned-out staff, and deferred revenue.
Your North Star Metric (NSM) should reflect this reality. Therefore, pick a single enterprise outcome that connects AI to value (e.g., clinician hours reclaimed or percent of documentation automated and error-free), and make it visible weekly. In this way, a North Star keeps cross-functional teams aligned on outcomes, not activity metrics.
If an AI initiative doesn’t give minutes back (soon) or measurably reduce a bottleneck (time-to-diagnosis, time-to-treatment, time-to-cash), it belongs in discovery, not in your 90-day capital plan.
2) Start where minutes compound: four wedge use cases
A) Ambient clinical documentation (GenAI + speech + NLP)
It attacks the universal bottleneck, documentation, without changing clinical decision rights.
Peer-reviewed studies in JAMA Network Open associate ambient scribe tools with greater clinician efficiency, lower mental burden of documentation, and higher patient engagement in outpatient care. KLAS created a dedicated Ambient Speech category, citing measurable gains in satisfaction, documentation quality, and efficiency.
What to measure: Reduction in minutes per note, after-hours EHR time, note accuracy on specialty templates, and patient-experience signals.
B) Prior authorization & revenue-cycle automation (RPA + rules + GenAI)
Low clinical risk, high administrative drag; automates a major cause of delays and write-offs.
Multi-partner deployments from Surescripts report approvals in ~30 seconds for in-scope medications, 88% fewer appeals, and large drops in denials due to missing information. Strong indicators of reclaimed care-team time and faster therapy starts (vendor data; validate in your environment).
What to measure: Cycle time from order to decision, avoidable denials, abandoned requests, and staff hours reallocated to exceptions.
C) Imaging triage and productivity (Computer Vision)
Concentrated specialist bottlenecks; CV can safely reduce low-value reads and accelerate critical pathways.
In screening mammography, randomized and real-world evidence show large workload reductions with similar cancer detection, freeing subspecialist minutes without compromising safety. In stroke, AI-enabled large-vessel occlusion (LVO) detection is associated with faster thrombectomy timelines in real-world analyses. Regulatory momentum is robust; the FDA’s public list of AI-enabled medical devices continues to expand, with radiology leading.
What to measure: Time-to-diagnosis, door-to-treatment, percent normal auto-cleared, and specialist throughput.
D) Predictive operations (Predictive analytics + ML)
Minutes saved upstream ripple through access and overtime; these tools operate on data you already generate.
A growing literature demonstrates accurate ED crowding and wait-time forecasts using ML, supporting proactive staffing and flow decisions; prospective and retrospective studies show reliable next-hour/next-day predictions and operational feasibility (impact depends on execution, tie predictions to staffing and bed-flow actions).
What to measure: forecast accuracy, wait times, LWBS (left without being seen), overtime, and patient throughput.
3) The healthcare AI toolbox. Deployed for time, not novelty in AI in healthcare transformation
Most organizations own the components already. The difference is in sequencing and measurement:
- AI/ML for forecasting demand, triage, and next-best action.
- Generative AI for structured documents and communication under human review.
- Computer Vision for high-volume image triage and quality assurance.
- Robotics & RPA for deterministic, repetitive workflows (pharmacy, revenue cycle).
- NLP to unlock the ~80% unstructured data (notes, voice, PDFs) trapped in your systems.
- Predictive Analytics to surface tomorrow’s bottlenecks today.
Treat unstructured data as a first-class asset. Quality, lineage, consent, and access are non-negotiable, or your models (and trust) will fail.
4) Governance for AI in healthcare transformation that runs weekly, not by quarterly panic
Transformation dies in the gap between ambition and execution. Consequently, the operating model that scales AI has clear decision rights, a weekly rhythm, and a non-negotiable model and business metrics on one dashboard.
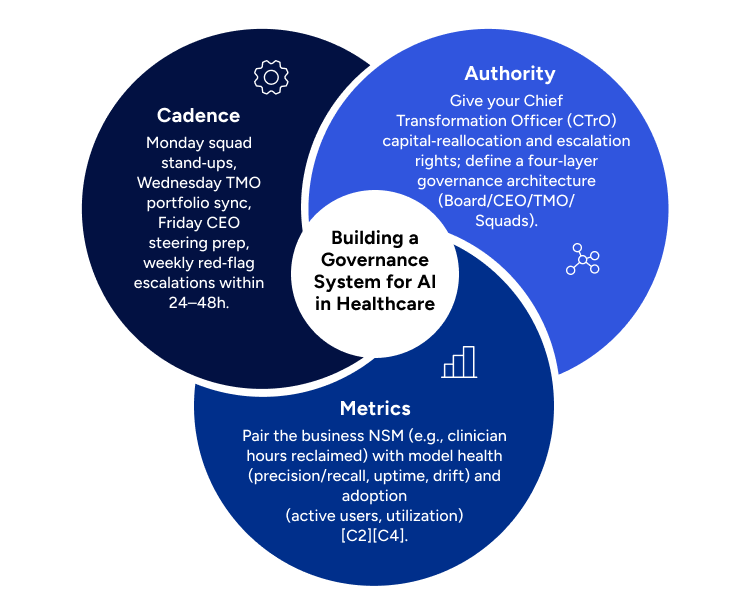
- Authority: Give your Chief Transformation Officer (CTrO) capital-reallocation and escalation rights; define a four-layer governance architecture (Board/CEO/TMO/Squads).
- Cadence: Monday squad stand-ups, Wednesday TMO portfolio sync, Friday CEO steering prep, weekly red-flag escalations within 24–48h.
- Metrics: Pair the business NSM (e.g., clinician hours reclaimed) with model health (precision/recall, uptime, drift) and adoption (active users, utilization).
Leaders are rightfully demanding ROI. The CTrO’s “Profit Guardian” mandate ties initiatives to the P&L, with CFO-validated baselines and rapid interventions when benefits slip.
Successful governance isn’t just technical, it’s organizational. Therefore, executives need a repeatable way to align teams, reallocate capital, and manage adoption. A structured Change Management Plan Template can accelerate alignment and reduce execution risk.
5) Data as a strategic asset
AI cannot change care without governed, high-quality, accessible data. In healthcare, unstructured content dominates, and poor data hygiene is a systemic risk to safety, trust, and ROI. Build pipelines that:
- Ingest and tag voice/text at source,
- Protect PHI by design (consent, minimization, auditability),
- Preserve raw and structured views (lineage), and
- Instrument quality and drift monitoring from day one.
Before scaling, assess your readiness. Consultport offers Digital Readiness Assessment and Digital Transformation Toolkit that help leadership baseline capabilities quickly and stand up execution assets without delay.
Regulatory momentum helps, but it raises the bar. Your models must be explainable, resilient, and aligned to HIPAA/GDPR. The FDA’s growing device list is a useful signal of what “good enough for the clinic” looks like.
6) A 90-day, outcome-first sequence for AI in healthcare transformation
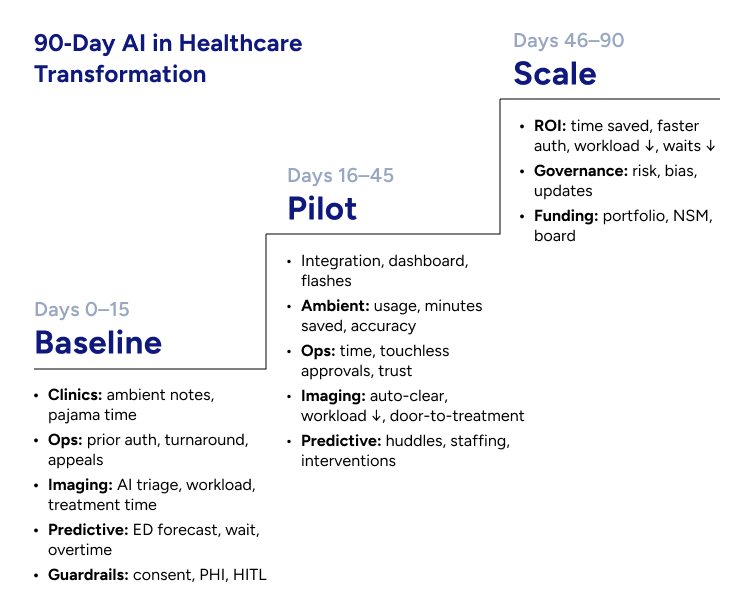
Days 0–15 — Pick wedge use cases and baseline rigorously
- Clinics: Launch ambient documentation in 2–3 specialties with consistent workflows (primary care, cardiology, pediatrics). Baseline minutes per note and after-hours EHR time (“pajama time”).
- Ops: Stand up prior-auth automation for a targeted medication class with payer/PBM alignment; baseline turnaround time and appeals.
- Imaging: Add AI-assisted triage to one high-volume pathway (mammography screening or LVO stroke alerts). Baseline reading workload and time-to-treatment.
- Predictive: Turn on an ED arrivals/occupancy forecast connected to staffing huddles; baseline wait times, LWBS, and overtime.
- Guardrails: Confirm consent flows, PHI controls, lineage, and human-in-the-loop review before go-live.
Days 16–45 — Pilot like you mean to scale
- Integrate with EHR/PACS; light up a single live dashboard for NSM, adoption, and model health; publish weekly flashes (green/yellow/red) by initiative.
- For ambient notes, track % of visits using ambient, minutes saved per note, and error-free automation rate; expand templates specialty-by-specialty.
- For prior auth, track median time-to-decision, % touchless approvals, and appeals; publish provider testimonials to build trust.
- For imaging, track % normals auto-cleared, reading workload reduction, and door-to-puncture/biopsy, where applicable.
- For predictive ops, run daily huddles to translate forecasts into staffing and bed-flow actions; log interventions and effects.
Days 46–90 — Lock ROI and codify the playbook
- Target outcomes supported by evidence and market data. Ambient notes saving minutes per encounter and reducing documentation burden; prior auth decisions in ~30 seconds for eligible meds; CV reducing imaging workload and accelerating critical care; predictive ops cutting waits and overtime.
- Publish a governance runbook (risk, bias, incident response, model updates) that generalizes to your next ten use cases.
- Seek portfolio funding only after the NSM moves; your board will back what performs, not what promises.
7) What the board will ask, and how to answer
“Is this hype or real?” Bain finds 54% of healthcare leaders already see meaningful ROI within the first year of GenAI initiatives. Pair that with the FDA’s expanding list of authorized AI-enabled devices. This is operational, not experimental.
“Will clinicians accept it?” JAMA Network Open studies associate ambient documentation with lower burden and higher engagement; KLAS’s dedicated report underscores adoption momentum and satisfaction.
“Does it move clinical/operational outcomes?” Mammography AI shows large workload reductions at similar detection; stroke LVO software is tied to faster treatment times; prior-auth automation collapses turnaround from hours to seconds in pilots (your numbers may vary, instrument and verify locally).
“What about risk?” Treat data as a strategic, governed asset; pair business KPIs with model health metrics; use a weekly cadence and clear decision rights to catch drift, bias, or safety signals early.
8) Scorecard: what “good” looks like in 12 weeks
North Star Metric (choose one):
- Clinician hours reclaimed (per week, per clinic); or
- % of documentation automated, error-free (by specialty).
Operational: after-hours EHR time ↓; time-to-diagnosis ↓; door-to-treatment ↓; throughput ↑; overtime ↓.
Clinical: maintained or improved detection/triage performance; safety events zero; audit pass rate 100%.
Adoption: active users; utilization per clinic day; specialty template coverage.
Model & platform health: precision/recall; latency/uptime; drift; PHI leakage tests.
Governance: consent coverage; decision-rights adherence; weekly flash compliance.
9) The strategic payoff of a time-first roadmap
When you start with time, you do more than rescue clinicians from keyboards. You build an execution system that turns AI from promise into performance:
- Capacity without new buildings: reclaimed minutes yield more appointments and shorter waits, fast.
- Trust by design: human-in-the-loop + transparent metrics build durable clinician and patient confidence.
- Reuse everywhere: the same data scaffolding and governance scale to imaging, prior auth, coding support, discharge planning, and beyond.
- Board-ready ROI: you show impact weekly, tied to P&L and patient access. That unlocks portfolio funding.
Momentum is on your side. Leaders report year-one ROI, regulators are signaling paths to safe scale, and ambient documentation has crossed from pilot to category. Ultimately, the winners will look “boring” before they look brilliant: fewer keystrokes, faster reads, shorter queues.
Is your organization ready to invert the roadmap by funding minutes, not models?
If so, Consultport connects providers, payers, and medtech firms with experienced AI consultants who bring governance playbooks, change-management expertise, and proven operating models to deliver measurable ROI in 90 days.
Executive FAQ
• What is “ambient clinical documentation”?
A system that converts clinician–patient conversations into draft notes for clinician review and sign-off (GenAI + speech/NLP), reducing manual EHR entry.
• Where does AI free time fastest?
Documentation (ambient notes), prior authorization/RPA, imaging triage, and predictive operations (staffing/ED flow).
• Is there evidence beyond pilots?
Yes. Peer-reviewed studies link ambient tools to lower documentation burden and higher efficiency; imaging AI shows large workload reductions with maintained detection; FDA approvals continue to rise, led by radiology.
• What should we measure first?
Clinician hours reclaimed, minutes per note, after-hours EHR time, door-to-diagnosis/treatment, and percent touchless prior-auth approvals.
• What safeguards matter most?
Consent, PHI minimization, lineage, human-in-the-loop review, model-health metrics, and a weekly governance cadence.
on a weekly basis.


